Seborrheic dermatitis (SD) is a very common, chronic inflammatory skin condition that can affect people of all ages. Often simply called dandruff when it’s on the scalp, it is characterized by greasy, yellowish scales on a background of redness. It’s not contagious, but it can be frustrating and recurring, often flaring up during periods of stress or cold, dry weather.
What Causes Seborrheic Dermatitis?
While the exact cause is not fully understood, SD is believed to be a combination of factors related to the skin’s oil production and immune response:
- Malassezia Yeast: An overgrowth of a normal skin yeast called Malassezia (also known as Pityrosporum ovale) is a major factor. This yeast thrives in oil-rich environments.
- Excess Sebum Production: The condition tends to occur in areas of the body that have a high concentration of sebaceous (oil-producing) glands.
- Inflammation: The body’s immune reaction to the overgrowth of Malassezia leads to inflammation, redness, and rapid skin cell turnover.
- Other Factors: Stress, fatigue, cold weather, and certain neurological or immune system disorders can also act as triggers.
Where Does Seborrheic Dermatitis Appear?
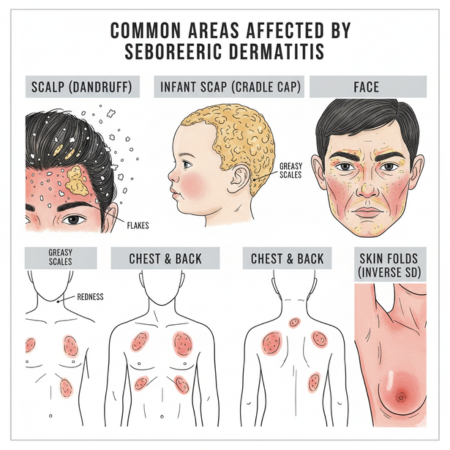
SD typically affects areas rich in oil glands, including:
- Scalp: Causing dandruff (white, powdery flakes) or, in severe cases, thick, greasy, yellowish scales. In infants, this is called cradle cap.
- Face: Especially around the eyebrows, the creases next to the nose (nasolabial folds), the forehead, and the ears (behind and in the ear canal).
- Chest and Back: Particularly the upper torso where patches of scaling can occur.
- Skin Folds: Areas like the underarms, groin, and under the breasts (Inverse or Flexural SD).
Here is a visual representation of common areas affected by Seborrheic Dermatitis:
Symptoms of Seborrheic Dermatitis
Symptoms can vary in severity but commonly include:
- Flaking skin (dandruff) on the scalp, hair, eyebrows, beard, or mustache.
- Patches of greasy skin covered with flaky white or yellowish scales, especially on the scalp, face, sides of the nose, eyebrows, ears, eyelids, and chest.
- Red skin.
- Itching.
- Burning or soreness.
Treatment and Management
While SD is a chronic condition, its symptoms can be effectively managed with various treatments. The goal is to reduce yeast growth, control inflammation, and remove scales.
- Medicated Shampoos, Creams, and Ointments:
- Antifungals: Shampoos or creams containing ketoconazole, selenium sulfide, or zinc pyrithione help control Malassezia yeast.
- Corticosteroids: Topical creams or lotions can quickly reduce redness and itching during flare-ups. Use under medical guidance due to potential side effects.
- Calcineurin Inhibitors: Pimecrolimus and tacrolimus creams can be effective, especially for sensitive facial areas.
- Salicylic Acid, Coal Tar, or Resorcin: Found in shampoos and lotions to help loosen and remove scales.
- Lifestyle and Home Remedies:
- Regular Washing: Wash affected areas frequently with a gentle cleanser. For the scalp, use medicated shampoos as directed.
- Moisturize: Use a light, non-comedogenic moisturizer, especially on facial areas, to prevent dryness from treatments.
- Avoid Irritants: Steer clear of harsh soaps, alcohol-based products, and anything that can dry out or irritate your skin.
- Manage Stress: Stress can trigger flare-ups, so finding healthy ways to manage it can be beneficial.
- Sunlight Exposure: Limited exposure to natural sunlight might help some individuals, but always protect your skin from sunburn.
- When to See a Specialist:
If over-the-counter treatments aren’t providing relief, or if your symptoms are severe, persistent, or causing discomfort, it’s advisable to consult a dermatologist. They can provide an accurate diagnosis, rule out other conditions, and recommend stronger prescription treatments.
Dr. Fahad Faizullah MBBS (KMC) – FCPS (Dermatology) Book An Appointment Call or WhatsApp +92 333 9352323 Timing: Monday to Friday 05:00 PM to 07:30 PM
