Acne Vulgaris is arguably the most common dermatological condition, affecting nearly everyone at some point in their lives, particularly during adolescence. Far from being a mere cosmetic issue, its impact can profoundly affect a person’s self-esteem, mental health, and quality of life. As a chronic inflammatory disease of the pilosebaceous unit (the hair follicle and its associated sebaceous gland), understanding this condition is the first step toward effective management and achieving clear, healthy skin.
Dr. Fahad Faizullah is a highly experienced dermatologist specializing in the diagnosis and advanced acne treatment of conditions like Acne Vulgaris. This in-depth resource is designed to educate patients on the complexities of this condition, from its underlying causes to the most advanced therapeutic strategies, including how to tackle challenging manifestations like cystic acne and the resulting acne scars.
Table of Contents
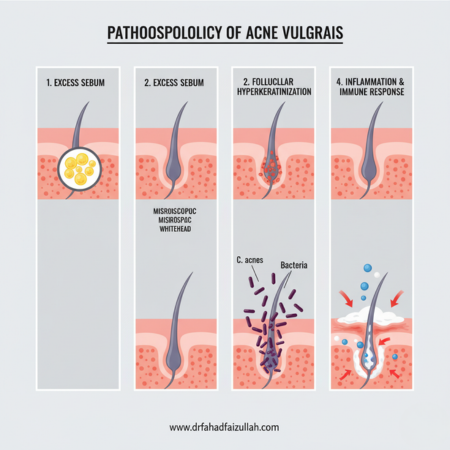
Understanding the Condition: Pathogenesis and Core Causes
To effectively treat this common skin disorder, one must first appreciate the intricate biological processes that lead to its development. The pathogenesis is multifactorial, involving an interplay of four primary, interconnected processes within the pilosebaceous unit.
1. Excess Sebum Production (Seborrhea)
The sebaceous glands, which are most abundant on the face, back, and chest, produce sebum—an oily substance vital for lubricating the skin and hair. The primary driver of increased sebum production is the surge in androgen hormones (like testosterone and DHEA) during puberty. Even in individuals with normal androgen levels, the sebaceous glands may be hypersensitive to these circulating hormones, leading to an overproduction of oil, a condition known as seborrhea. This excess sebum creates an ideal, lipid-rich environment within the hair follicle, a crucial precursor to the inflammation.
2. Follicular Hyperkeratinization
Normally, dead skin cells (keratinocytes) are shed and expelled from the pore. In those with the condition, this process becomes defective. The cells lining the hair follicle, instead of shedding normally, stick together, leading to a buildup that clogs the follicular opening. This phenomenon, called follicular hyperkeratinization, results in the formation of a microcomedone—the microscopic, foundational lesion. When this blockage is complete, it forms a whitehead (closed comedones); when it’s partially open to the surface, the trapped mixture oxidizes, forming a blackhead (open comedones).
3. Proliferation of Cutibacterium acnes (C. acnes)
Cutibacterium acnes (previously known as Propionibacterium acnes) is a type of bacteria that naturally resides on the skin. It is an anaerobe, meaning it thrives in low-oxygen environments. The clogged, sebum-rich follicle creates a perfect, oxygen-depleted breeding ground, allowing C. acnes to multiply rapidly. The bacteria metabolize the components of sebum into inflammatory byproducts.
4. Inflammation and Immune Response
The accumulation of sebum, keratinocytes, and the byproducts of C. acnes within the follicle triggers a potent inflammatory response from the body’s immune system. White blood cells are deployed, leading to the characteristic redness, swelling, and pain of inflammatory lesions. This inflammation ranges from small papules and pustules to deep, painful nodules and cysts, the hallmarks of severe breakouts.
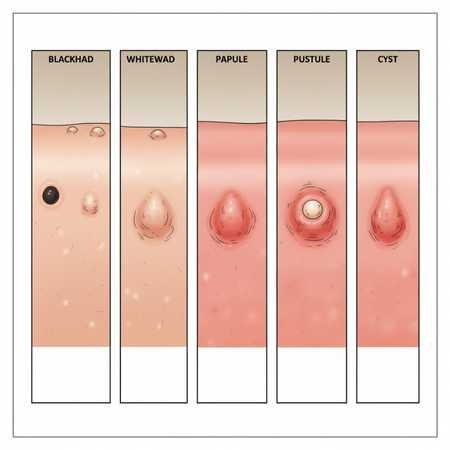
Types and Severity of Skin Lesions
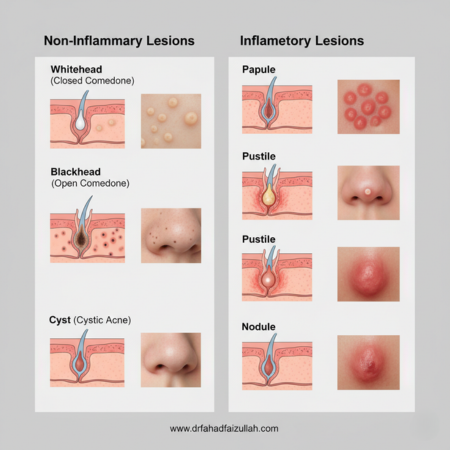
Acne Vulgaris manifests in various forms, and acne treatment strategies are heavily dependent on correctly identifying the type and severity of the dominant lesions.
Non-Inflammatory Lesions (Comedones)
These are the earliest and mildest forms of the skin condition.
- Whiteheads (Closed Comedones): Small, flesh-colored or whitish bumps. The follicle is completely plugged, trapping the contents beneath the skin surface.
- Blackheads (Open Comedones): The pore is partially open, allowing the trapped sebum and dead cells to oxidize upon exposure to air, resulting in a dark appearance.
Inflammatory Lesions
These lesions signify a rupture of the follicle wall, releasing contents into the surrounding skin, and initiating an immune response.
- Papules: Small, tender, raised, red bumps. They do not have a visible pus head.
- Pustules: Commonly referred to as “pimples,” these are red, inflamed spots with a visible white or yellow centre of pus at the tip.
Severe Inflammatory Lesions: Nodules and Cysts
These represent the most severe forms of the disorder, often resulting in significant pain and a high risk of permanent acne scars.
- Nodules: Large, hard, painful lumps that form deep beneath the skin surface. They are the result of severe inflammation and deeper follicular rupture.
- Cysts (Cystic Acne): These are the most extreme lesions—large, soft, pus-filled lumps that resemble boils. Cystic acne is exceptionally painful, destructive, and requires prompt, aggressive medical acne treatment to prevent disfigurement. The term cystic acne is sometimes used interchangeably with nodular acne, but both signify severe disease.
Factors That Trigger or Worsen Acne
While the four primary mechanisms above are the direct causes, several external and internal factors can trigger or exacerbate episodes.
1. Hormonal Fluctuations (Hormonal Acne)
Hormones are a paramount factor, particularly in this condition affecting adolescents and adult women.
- Puberty: The natural surge of androgens initiates the breakout process.
- Menstrual Cycle: Many women experience pre-menstrual flares of hormonal acne due to monthly shifts in estrogen and progesterone levels.
- Pregnancy and Menopause: Both periods involve significant hormonal shifts that can either trigger or resolve breakouts.
- Endocrine Conditions: Conditions like Polycystic Ovary Syndrome (PCOS) are characterised by androgen excess and frequently present with challenging hormonal acne.
2. Diet and Lifestyle
The role of diet in skin health remains a topic of research, but evidence suggests two main areas of concern:
- High Glycemic Index (GI) Foods: Foods that cause a rapid spike in blood sugar (e.g., white bread, sugary drinks, processed foods) may promote the release of insulin-like growth factor-1 (IGF-1), which in turn stimulates sebum production and exacerbates breakouts.
- Dairy Products: Particularly skim milk, has been linked to an increased risk, potentially due to their hormonal content.
- Stress: While stress doesn’t directly cause acne, it can worsen existing conditions by increasing cortisol and other stress-related hormones, which may stimulate the sebaceous glands. For more clinical information on stress and skin disorders, you can refer to resources like the National Center for Biotechnology Information (NCBI). [Outbound Link to NCBI/PubMed on Stress and Skin]
3. Medications and Cosmetics
- Medications: Certain drugs, including corticosteroids, lithium, and some anti-epileptic medications, are known to induce or worsen skin breakouts.
- Comedogenic Products: Heavy or oily skincare products and makeup can clog pores, creating new comedones and contributing to the cycle of breakouts.
The Comprehensive Acne Treatment Approach
Effective acne treatment is not one-size-fits-all. Dr. Fahad Faizullah employs a stratified approach based on the type and severity of lesions, focusing not only on clearing current breakouts but also on preventing new ones and minimising the risk of acne scars.
1. Treatment for Mild Acne Vulgaris (Comedonal Acne)
Mild Acne Vulgaris, primarily consisting of comedones (blackheads and whiteheads), is generally managed with topical therapies.
- Topical Retinoids (e.g., Tretinoin, Adapalene, Tazarotene): These are the cornerstone of Acne Vulgaris treatment. They normalize follicular keratinization, helping to unplug comedones and prevent the formation of new ones. Adapalene is often favoured as a first-line therapy due to its better tolerability.
- Salicylic Acid and Alpha Hydroxy Acids (AHAs): These act as chemical exfoliants, helping to shed dead skin cells and clear clogged pores. Salicylic acid (a Beta Hydroxy Acid) is particularly effective for penetrating oily pores.
- Azelaic Acid: This agent has anti-bacterial, anti-inflammatory, and comedolytic properties, making it an excellent option, especially for patients who cannot tolerate retinoids or as a safe option during pregnancy.
2. Treatment for Moderate Acne Vulgaris (Papules and Pustules)
Moderate Acne Vulgaris, characterised by papules and pustules, typically requires a combination therapy to address the multiple underlying causes (bacteria, inflammation, and follicular clogging).
- Topical Combination Therapy: Often involves combining a topical retinoid (for comedones and prevention) with an antimicrobial/anti-inflammatory agent.
- Benzoyl Peroxide (BPO): A powerful antimicrobial that kills C. acnes bacteria and also has comedolytic properties. Crucially, bacteria do not develop resistance to BPO, making it an essential partner for antibiotics.
- Topical Antibiotics (e.g., Clindamycin, Erythromycin): Used in combination with BPO to reduce C. acnes populations and inflammation. They should never be used alone due to the risk of bacterial resistance.
- Oral Antibiotics (e.g., Doxycycline, Minocycline, Sarecycline): For widespread or deeper inflammatory lesions, systemic antibiotics are prescribed for a limited duration (typically 3-4 months). They target the bacteria and provide a strong anti-inflammatory effect.
3. Treatment for Severe Acne Vulgaris (Nodules and Cystic Acne)
Severe Acne Vulgaris, involving nodules and cystic acne, often requires the strongest available therapies to prevent permanent acne scars and psychological distress.
- Oral Isotretinoin (Accutane): This is a highly effective, powerful retinoid derivative reserved for severe, nodular, or therapy-resistant Acne Vulgaris. It is the only treatment that targets all four causes of Acne Vulgaris by drastically reducing sebum production, normalizing keratinization, and indirectly reducing C. acnes. Due to potential side effects and the risk of severe birth defects (teratogenicity), its use requires strict patient monitoring, typically managed only by a specialist like Dr. Fahad Faizullah.
- Hormonal Therapy (Hormonal Acne): For women with classic hormonal acne patterns, therapies that modulate androgen activity can be highly effective.
- Combined Oral Contraceptives (COCs): Certain birth control pills help regulate hormones and reduce sebum production.
- Spironolactone: An anti-androgen medication used to treat hormonal acne in women by blocking the effect of androgens on sebaceous glands.
- Intralesional Corticosteroid Injections: For individual, particularly painful, large nodules or cysts (cystic acne), an injection of a corticosteroid can rapidly reduce inflammation, pain, and the likelihood of scarring.
Dealing with the Aftermath: Acne Scars and Pigmentation
A significant concern for patients with Acne Vulgaris, especially those with a history of severe inflammation or cystic acne, is the potential for long-term skin changes. These after-effects fall into two main categories: post-inflammatory hyperpigmentation (PIH) and true acne scars.
Post-Inflammatory Hyper- or Hypopigmentation (PIH)
These are temporary color changes in the skin after an inflammatory lesion heals.
- Hyperpigmentation: Dark spots (red, purple, or brown) where a pimple once was. This is an overproduction of melanin in response to inflammation. It is not a true scar and typically fades over time, though topical agents like hydroquinone, retinoids, azelaic acid, and vitamin C can accelerate clearance.
- Hypopigmentation: Light spots, though less common, can also occur.
True Acne Scars
These represent permanent changes in the skin texture due to abnormal collagen production during the healing process of deep, inflammatory lesions.
- Atrophic Scars (Depressed): Caused by a loss of tissue.
- Ice Pick Scars: Narrow, deep, V-shaped pits.
- Boxcar Scars: Broad, sharp-edged depressions.
- Rolling Scars: Broad, shallow depressions that give the skin a wavy, undulating appearance.
- Hypertrophic/Keloid Scars (Raised): Caused by an overgrowth of tissue, most common on the chest and back.
Advanced Acne Scar Treatment Options by Dr. Fahad Faizullah
Dr. Faizullah offers a range of sophisticated treatments tailored to the type of acne scars:
- Chemical Peels (e.g., TCA, Jessner’s): Used to exfoliate the top layers of skin, improving texture and mild scarring.
- Microneedling (Collagen Induction Therapy): Stimulates collagen production to fill in atrophic acne scars.
- Laser Resurfacing (e.g., Fractional CO2): Uses light energy to remove damaged outer skin layers and stimulate deep collagen remodelling.
- Subcision: A technique used to break up the fibrous bands that tether rolling acne scars down, allowing the skin to rise.
- Dermal Fillers: Used to immediately raise deep, depressed scars.
- Surgical Punch Excision/Grafting: For deep ice pick scars.
Maintaining Clear Skin: Long-Term Management of Acne Vulgaris
The treatment of Acne Vulgaris is a marathon, not a sprint. Once initial breakouts are controlled, a maintenance phase is crucial to prevent recurrence, which is common with conditions driven by hormones and genetics.
Skincare Routine Essentials for Acne Vulgaris
- Gentle Cleansing: Wash the affected areas (face, chest, back) twice daily with a mild, pH-balanced, non-comedogenic cleanser. Aggressive scrubbing or harsh soaps can worsen inflammation.
- Consistency with Topicals: Continue to use a topical retinoid (such as Adapalene) regularly, even when the skin is clear. This is the best defense against new comedones.
- Sun Protection: Many acne treatment medications, particularly topical retinoids and oral antibiotics, increase sun sensitivity. Daily use of a non-comedogenic, broad-spectrum sunscreen is essential to prevent sunburn and the darkening of post-inflammatory hyperpigmentation.
- Avoidance: Avoid picking, squeezing, or popping lesions. This trauma forces debris deeper into the skin, drastically increasing the risk of inflammation, infection, and permanent acne scars and hyperpigmentation.
When to Consult a Dermatologist for Acne Vulgaris
It’s time to see a specialist if over-the-counter products fail to improve your skin after 6-8 weeks, if you are experiencing cystic acne or large, painful nodules, or if you are developing acne scars or significant PIH. A board-certified dermatologist like Dr. Fahad Faizullah can accurately diagnose your specific type of Acne Vulgaris, discuss systemic acne treatment options like oral antibiotics or isotretinoin, and initiate advanced procedures for scar revision.
Acne Vulgaris is a complex, chronic condition that demands expert care. By understanding the causes—from excess sebum and clogged comedones to the deep inflammation of cystic acne—Dr. Fahad Faizullah develops personalized acne treatment plans. The goal is always to clear the skin, manage hormonal acne triggers, prevent the formation of new lesions, and provide effective solutions for minimizing and treating existing acne scars.
Dr. Fahad Faizullah: Your Partner in Skin Health
Dr. Fahad Faizullah is committed to providing the highest standard of evidence-based dermatological care. If you are struggling with persistent Acne Vulgaris, severe inflammation, or looking for advanced solutions for acne scars, book a consultation to discuss a comprehensive and personalised acne treatment plan.
Dr. Fahad Faizullah MBBS (KMC) – FCPS (Dermatology) Book An Appointment Call or WhatsApp +92 333 9352323 Timing: Peshawar Monday to Wednesday and Friday 05:00 PM to 07:30 PM Timing: Kohat Clinic Sunday 10:00 AM to 03:00 PM Timing: Swabi Clinic Thursday 10:00 AM to 04:30 PM www.drfahadfaizullah.com